
Department of Otolaryngology, Head and Neck Surgery
 |
Otology Department of Otolaryngology, Head and Neck Surgery |
| Home | Unit One | Unit Two | Unit Three | Unit Four | Unit Five | Unit Six | Unit Seven | Unit Eight | References |
Four conditions of the external ear including external otitis, canal and tympanic membrane trauma, and impacted cerumen are covered in this section.
External otitis pertains to all the inflammatory processes that change the continuity of the epithelium of the external auditory canal, meatus, and tympanic membrane skin. There are at least four types of external otitis: Bacterial, Fungal, Eczematoid and Viral.
History:
This is a 35 year old man with ear pain that began 48 hours ago. The pain is severe, constant and is worse with chewing. No history of previous ear disease.
Examination:
Notice the swelling of the external canal. The canal has become erythematous and edematous, with occlusion of the meatus. The opening to the canal can also have whitish debris and serous drainage that appears yellow in color.
 |
|
| ^Click on the arrow to view the video |
Information: Bacterial external otitis may be acute or chronic and it may be localized to a small portion of the canal or diffuse with cellulitis and extending to the outer ear, parotid region, and posteriorly to the skin overlying the mastoid.
It is usually caused by Pseudomonas aeruginosa and Staphylococcus aureus.
Signs and symptoms include pruritis in the external ear, pain, discomfort with jaw motion, foul-smelling, greenish-yellowish drainage, fever, possible conductive hearing loss, edema, and erythema of canal skin. Patients usually have a recent history of water activity or ear cleaning. If untreated, the infection can spread to the cartilage and bone surrounding the ear canal causing cellulitis.
Bacterial infection is frequently called "Swimmer's Ear" because of it's cause by ear wetness. It can occur as a sole diagnosis or may be seconday to otitis media with a lot of drainage through a tympanic membrane perforation. The otorrhea will cause the external otitis. An acute external otitis frequently complicates a previously untreated skin condition of the external canal. In an immunocompromised patient or poorly controlled diabetic, if left untreated it may lead to necrotizing (previously termed malignant) external otitis with cellulitis. The predominent organism is usually Pseudomonas aeruginosa.
Treatment is with antibiotic/antibiotic steroid drops, local debridement and possible wick placement depending on the severity. The wick is inserted into the edematous canal and then soaked with drops to expand. Drops are continued for about 3 days with the wick in place. The wick is then removed, and the drops are continued for several more days.

External otitis: FungalHistory: Examination:
|
|
 |
|
| ^ Click on the arrow to view the video | |
 |
 |
Information: Fungus is frequently the cause of inflammatory external otitis.Fungal infection: An infection in which fungi grow in the canal causing superficial redness of the bony canal wall skin with musty smelling exudate and powdery appearing debris (fungal mycelia). Moisture and immunosuppresion increase the incidence of this otitis. |
|
History: This is a 55 year old man who presents to the clinic for itching in his ear. This pruritis has been present for many years, but it has been increasing over the last 6 months.
Examination: The dry flaking and scaling of the external canal can usually be seen in the external ear as it leads into the external canal. The bony portiion of the external canal is normal and the tympanic membrane is normal.
 |
There is no video associated with this picture. |
Information: Eczematoid There are many types of eczematoid otitis. Most start as a dry, flaking, and scaling condition. The ear dermatitis is frequently associated with scalp and facial lesions.
History:
This 35 year old female presented to the clinic with one day's duration of severe pain and a total facial palsy on the right side. She was sent home on steroids with a diagnosis of Bell's palsy. She returned 4 days later with these painful vesicles on her concha and external ear canal.
Examination:
Upon examination of the right ear, the vesicles are evident. Some may be ruptured with the erythematous margin surrounding them.
 |
 |
Information: Herpes Zoster Oticus is a viral infection of the geniculate ganglion and other cranial nerve ganglia. It is caused by reactivation of varicella-zoster virus (VZV). Frequently it is called Ramsey Hunt syndrome when the rash is accompanied by facial paralysis indicating that the virus has spread to the facial nerve.
The chief symptom is severe pain in the ear that may precede physical findings by several days. The typical physical findings are herpetic vesicles on the concha and external ear canal and /or facial nerve palsy. Since the virus can affect the VII, VIII, or IX cranial nerves, symptoms of hearing loss,and dizziness accompanied by nausea and vomiting are common.
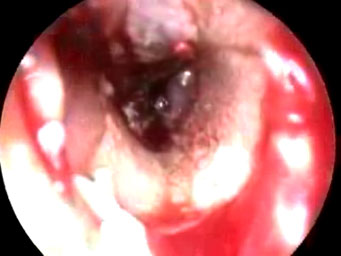
Examination:
Notice the blood in the external canals and hemorrhagic clots adjacent to ruptured TM.
 | |
| ^ Click on the arrow to view the video |
Information: Canal trauma is an injury to the skin and/or the bony canal by accident. Direct trauma occurs when an object is inserted and damages the bony canal or skin of the auditory canal. Indirect trauma is caused by a head injury resulting in a longitudinal fracture of the temporal bone. Signs and symptoms include a ‘dull’ feeling, hearing loss, ossicular discontinuity, bloody discharge, and possible facial nerve weakness.
History:
This is a patient with recurrent cerumen impactions. The chief complaint is fullness and hearing loss.
Examination:
Note that the cerumen is removed with a curette from the canal wall towards the center of the canal to prevent injury to the canal skin.

|
^Click on the arrow to view the video |

|
^Click on the arrow to view the video |
Information: Impacted cerumen is the accumulation of cerumen in the external ear canal.The acidic pH of the secreted cerumen may inhibit bacterial growth in the canal. Some cerumen is needed, but excess accumulation blocks hearing. The accumulation of wax increases in patients who wear ear plugs and hearing aids.
Signs and symptoms include a ‘dull’ feeling in the ear, slight tinnitus, vertigo, autophony (hearing oneself speak), pain, acute myringitis, pressure sensation, and a dry cough.
Treatment involves softening and removing the wax with a curette, suctioning, or irrigation. These impactions can also be irrigated as long as the pateint does not have one of thethe following:
-tympanic membrane perforation
-a myringotomy tube
-a monomere (very thin ear drum)
-a mastoid cavity
-chronic external otitis.
A monomere can turn into a perforation; chronic external otitis can be made worse with the irrigation and irrigation of a mastoid cavity will make the patient very dizzy because of the proximity of the lateral/horizontal semicircular canal.
| Home | Unit One | Unit Two | Unit Three | Unit Four | Unit Five | Unit Six | Unit Seven | Unit Eight | References |
Site administrator:
Barbara
Heywood MD.
Copyright © 2014
 All rights reserved.
All rights reserved.