
Department of Otolaryngology, Head and Neck Surgery
 |
Otology Department of Otolaryngology, Head and Neck Surgery |
| Home | Unit One | Unit Two | Unit Three | Unit Four | Unit Five | Unit Six | Unit Seven | Unit Eight | References |
 |
|
| ^Click the arrow to view the video |
 |
|
| ^Click the arrow to view the video |

|
^ Click on the arrow to view the video |
 |
 |
Information: A bobbin tube is a bobbin-shaped tube that is inserted into the tympanic membrane to aid in the aeration/ventilation of the middle ear and maintain equal pressure when the Eustachian tube is not functioning. This tube typically stays in for six to twelve months and extrudes by itself.
 |
|
| ^Click the arrow to view the video |
 |
 |
Information: A T-tube is a ventilation tube, shaped like a ‘T’. A T-tube is inserted in the tympanic membrane to aerate/ventilate the middle ear and maintain equal pressure when Eustachian tube function isinadequate. This tube is often used when long-term ventilation is needed. T-tubes may extrude spontaneously, but often require office removal when they do not.
History:
This is a T tube that was inserted in the tympanic membrane a year ago for chronic serous otitis. The patient now presents with the complaint of intermittent bleeding from the ear.
Examination:
The tube is found to be surrounded by granulation tissue. An aural polyp can be seen anterior to the tube.
 | ^ Click on the arrow to view the video |
History:
This is a 50 year old female who presented for a post surgery visit. The patient had a hearing loss secondary to chronic otitis with the loss of her incus. She had surgery to insert a prosthesis to replace the ossicular chain.
Examination:
Notice the whitish area in the left ear drum. It is in the posterior section and appears as a thickening in the TM. The cartilage was used to separate the TM from the ossicular prosthesis to protect it from extruding.
 |
^ Click on the arrow to view the video |
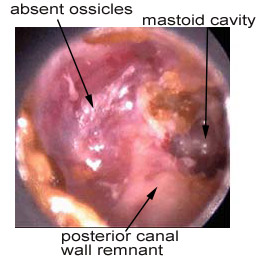
History:
This is a fifty year old female who has had multiple ear operations. She complains of decreased hearing. She has no drainage or pain. If she accidently gets cold water in her ear, it makes her very dizzy. She cannot have her ear cleaned by irrigation.
Examination:
Radical mastoid cavity - Notice the absence of a normal ear drum. Squamous epithelium covers the middle ear. There are no ossicles. The meatus of the external canal is much larger than normal and the mastoid cavity can be viewed behind the middle ear remnant through the external canal. A remnant of the posterior canal wall protrudes from the floor of the cavity, separating the middle ear remnant from the mastoid cavity.
 |
^ Click on the arrow to view the video |
Modified radical mastoidectomy cavity - The second set of pictures also shows a mastoid cavity, but the posterior canal wall is more prominent. The ossicles and tympanic membrane are also present. The superior portion of the ear canal has been removed at the level of the TM.
Information: A complete masoidectomy or simple mastoidectomy is the removal of the bony walls separating the mastoid air cells, leaving a large cavity. On physical exam, the scar from the postauricular incision can be seen. Often, a depressed area, corresponding with the cavity, can be seen. The TM may be very normal in appearance.
If only the lateral part of the canal wall is removed and the middle ear is spared, then the procedure is called a modified radical mastoidectomy. In these cases the ossicular chain can be reconstructed to preserve hearing. Potential complications of mastoidectomy include injury to the facial nerve, penetration of the middle fossa dura, rupture of the sigmoid sinus, and labyrinthine injury.
Radical mastoidectomy is a complete mastoidectomy plus the removal of the posterior canal wall and all remnants of the middle ear including the tympanic membrane, malleus, incus, tensor tympani muscle, and middle ear mucosa. This procedure is used in cases where the disease extends into the mastoid and middle ear cavity. Since this results in significant hearing loss, it is commonly reserved for especially severe disease and tumors involving the middle ear or the external canal.
 Modified radical mastoidectomy Modified radical mastoidectomy |
^ Click on the arrow to view the video | |
| Home | Unit One | Unit Two | Unit Three | Unit Four | Unit Five | Unit Six | Unit Seven | Unit Eight | References |
Site administrator:
Barbara
Heywood MD.
Copyright © 2014
 All rights reserved.
All rights reserved.