
Department of Otolaryngology, Head and Neck Surgery
 |
Otology Department of Otolaryngology, Head and Neck Surgery |
| Home | Unit One | Unit Two | Unit Three | Unit Four | Unit Five | Unit Six | Unit Seven | Unit Eight | References |
A perforation is a hole in the tympanic membrane that is visible through the otoscope. This section contains information on acute traumatic, central, marginal, attic, and total perforations along with information on the monomeric tympanic membrane.
History:
A 25 year old male was seen in the clinic for decreased hearing. The patient fell while waterskiing and immediately noticed a hearing loss accompanied by severe pain.
Examination:
The patient has a torn tympanic membrane. The perforation is linear.
 |
|
| ^ Click on the arrow to view the video |
Information: An acute traumatic perforation of the tympanic membrane is due to an impact to the head/ear or penetration of an object through the ear canal. For a perforation to occur, a pressure increase of 25 lb./sq.in. is required to the head. This may result in a temporal bone fracture, allowing leakage of cerebrospinal fluid into the middle ear space. Perforations due to instrumentation, such as Q-tips,and to fireworks and waterskiing accidents are common.They may cause a mild to moderate hearing loss, depending on the size of the perforation. The hearing loss is never severe because of the perforation alone. If severe deafness occurs, it is a sign of additional inner ear trauma. Perforations can also lead to infection and drainage. Most traumatic perforations heal spontaneously, usually within a month.
Signs andsymptoms include pain, bleeding, dysequilibrium/imbalance, and tympanic membrane perforation. The perforation usually heals spontaneously. A sound pressure levelof 195-199dB is required to cause a perforation in the tympanic membrane. An audiogram is required to discover disruption of the ossicles. Surgical intervention to realign the middle ear ossicles may be necessary if a discontinuity of the ossicles occurs.
History:
This is 30 year old male who came in with complaints of hearing loss, but no pain. Past medical history was positive for recurrent ear infections as a child and myringotomies with tube placement multiple times. His last ear examination was 10 years ago.
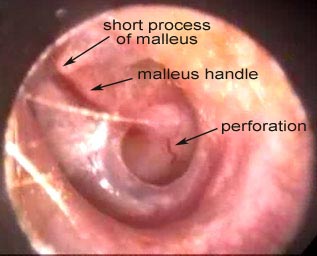
Examination:
This is a central perforation with a rim of intact TM around the edges of the perforation. The perforation is dry, no granulation tissue is seen, and the middle ear mucosa is normal.
 |
|
| ^ Click on the arrow to view the video |
Information: A central perforation is a perforation in the pars tensa that leaves an intact portion of the tympanic membrane between the rim of the perforation and the bony canal. The fibrous annulus, the tickened portion of the TM near the bony canal, is also intact. This perforation usually follows an upper respiratory infection or fluid in the middle ear. The handle of the malleus may project into the perforation.
Signs and symptoms may include a mild to moderate hearing loss if the perforation is large. Small perforations may be asymptomatic. Purulent otorrhea indicates superimposed infection or chronic otitis media. Complications include aural polyps, necrosis of the incus, and cholesteatomas.
History:A 55 year old male returns to the clinic because of hearing loss. He has a life-long history of repeated ear perforations and multiple ear surgeries.
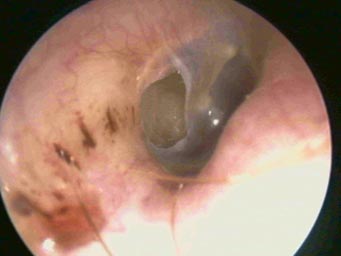
Examination:
The TM has a posterior marginal perforation in the pars tensa.
 | There is no video associated with this picture. |
Information: A marginal perforation is a perforation that has an area with no tympanic membrane between the perforation and the bony canal. Because of this, squamous epithelium may grow into to the middle ear cavity. This perforation is often associated with a cholesteatoma but is usually the result of acute necrotizing otitis media destroying the annulus and mucous membrane. Usually it is seen posteriorly, meaning the perforation may have originated from a retraction pocket.
Signs and symptoms include conductive hearing loss and otorrhea. Complications are the same as for otitis media.
History:
This is an 89 year old woman who had suffered from scarlet fever as a child. She has had difficulty hearing most of her life. She has no pain and no drainage. Her audiogram indicates a severe to profound mixed hearing loss.
Examination:
Note the complete loss of the pars tensa of the TM. The middle ear mucosa appears normal.
 |
^ Click on the arrow to view the video |
Information: A complete absence of the tympanic membrane. The mallens is retracted medially and cannot be seen. Large perforations such as this occurred commonly with strep infections and chronic otitis media. They cause a moderate conductive hearing loss

History:
A 14 year old male is seen for a routine high school physical. He has no complaints. His father states that "he had ear infections as a child and had ruptured ear drums on several occasions". There was no problem with school hearing tests.
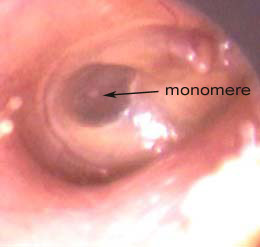
Examination:
Notice the transparent area posterior to the malleus. There is absence of the middle, fibrous layer resulting in the transparency. Frequently, this is mistaken for a perforation, but note that the middle ear space cannot be clearly seen. Pneumo-otoscopy can also be helpful to differentiate a monomere from a perforation.
The lower picture shows a monomere of a large area of the TM. It is extremely thin and moves with heavy respiration.
 |
|
| ^Click the arrow to view the video |
 |
|
| ^Click the arrow to view the video |
Information: A monomere is a area of thin, transparent tympanic membrane due to the absence of the dense fibrous layer. It usually occurs after a perforation. A monomere will not usually affect the audiogram. The tympanogram may be normal or show increased mobility with a higher peak at the normal pressure. Momomeres are usually not a problem unless the patient experiences severe and sudden pressure changes. They can perforate more easily than normal TM.
| Home | Unit One | Unit Two | Unit Three | Unit Four | Unit Five | Unit Six | Unit Seven | Unit Eight | References |
Site administrator:
Barbara
Heywood MD.
Copyright © 2014
 All rights reserved.
All rights reserved.